Treating Lipedema
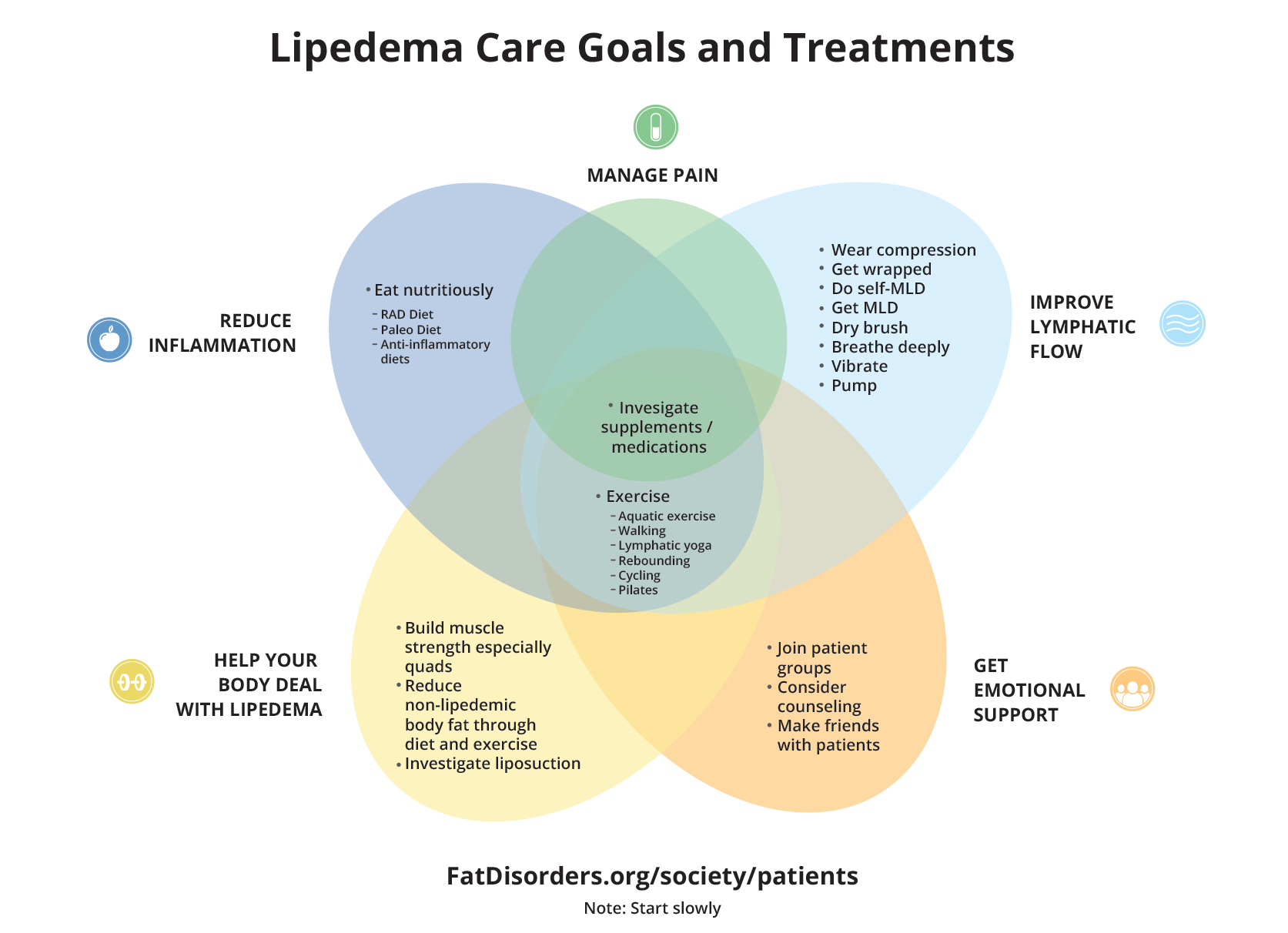
The goals of treating Lipedema are to: Reduce inflammation, manage pain, improve lymphatic flow, receive emotional support, and help the body deal with Lipedema. Many treatments can be done cheaply at home by the patients and are demonstrated and discussed on the FDRS Self-Care playlist on YouTube.
When considering treatments, keep in mind which are “conservative” meaning non-invasive, and which are invasive/surgical. In the US, many insurance plans require patients to attempt conservative treatments before they will consider coverage for invasive procedures.
Moreover, some surgeons will not operate unless a patient first establishes healthy routines with conservative treatments. Surgery may not correct the underlying issues, and patients will still need healthy conservative treatment habits after surgery.
Conservative Treatments
Conservative treatments can be thought of as lifestyle changes (better nutrition and more moderate exercise), mechanical (MLD, compression garments and compression pumps), and supplements/medications. Treatments that are cheap and easy to start include deep breathing, dry brushing and walking.
Therapy
A proof-of-principle study published in 2022 by Donahue et. al found that patients with early stage Lipedema could benefit from physical therapy to manage leg pain and improve quality of life. Nine 60-minute therapy sessions spanned a total of 6 weeks and included manual therapy, tailored exercise guidance for a home program, education and compression needs. Post-therapy, pain and function had clinically significant improvements and sodium levels in the skin and SAT regions had reduced, indicating lower inflammation in the treated areas. See more from that study here.
Seeing a therapist familiar with treating Lipedema, typically a Certified Lymphedema Therapist (CLT), can be helpful. These professionals usually consist of physical therapists, occupational therapists, and licensed massage therapists, and have typically received Lipedema-specific training.
Nutrition
Research surrounding nutrition for Lipedema is still evolving, and there is not much data to support one particular diet. Some diets that have been utilized in the field include: paleo, keto, LCHF (low carb high fat), RAD (rare adipose disorder diet), and anti-inflammatory. As Lipedema tissue is typically resistant to caloric restriction; it is generally suggested to utilize diet to lower overall inflammation and alleviate symptoms.
For many who are trying new diets to support their health, it can be helpful to take note of which foods may aggravate or relieve symptoms.
The Lymphedema and Lipedema Nutrition Guide book is a resource that helps people identify practicable changes to eat healthier foods that can support people with Lipedema and Lymphedema.
Exercise
Exercise recommendations are usually: walking, aquatic exercise of any kind, Pilates, cycling, and yoga. The goals are to get the lymphatic system moving, take care of your joints if you are hypermobile, and build strength to help combat extra weight.
CLTs can help develop a tailored exercise program designed to support patients with Lipedema.
Supplements
Certain vitamin and/or mineral deficiencies may present with Lipedema, and these deficiencies may warrant the use of supplements. Current research does not give a definitive answer on this subject. Patients should consult with a physician that can perform appropriate testing to assess the need for use of supplements and monitor use as needed.
Keep in mind that supplements are not tested by the FDA so there is no way to know about possible side effects. Most diuretics do not help alleviate the swelling of Lipedema.
Compression
Several recent studies have upheld compression as an effective non-surgical treatment modality. Both compression garments and pneumatic compression devices (pumps) can deliver benefits for quality of life and potential changes to body composition.
Compression garments should be tailored to the patient. There are many types, sizes, and strengths of compression garments and all of these factors will likely have an impact on how effective the garment is at reducing inflammation, pain, and swelling. For the best chance of finding appropriate compression garments, patients can work with an experienced therapist or compression fitter to ensure accurate fit.
Surgical Treatments
Lipedema patients often seek surgery in order to alleviate pain, increase mobility, decrease joint stress, and improve their quality of life.
The procedures most often considered for Lipedema patients include: Liposuction, vein surgery, knee and/or hip replacements, excisions of fat nodules, bariatric surgery to treat abdominal obesity*, and debulking/lifts/resections.
Whenever surgery is considered for Lipedema patients, the pre-op routine, surgical technique and post-op care should be very carefully tailored to the patient and the protocols can vary greatly by surgeon. Some surgeons advise their patients to develop healthy routines before surgery, especially incorporating healthy eating and exercise habits. Many surgeons and clinicians advise that surgeons should go to great lengths to avoid damaging shallow and deep lymphatics and vasculature in this patient group.
Many insurance plans require a trial of conservative treatments prior to covering surgical procedures. Individual insurance plans vary, so it is important to contact your insurance provider to gather more information.
Notes on Liposuction
Early liposuction techniques removed a lot of tissue without discriminating what gets removed; newer techniques focus on leaving the vasculature and lymphatic systems intact as much as possible.
Realistic expectations should be set with patients receiving liposuction as to aesthetic outcomes, which may vary. Many surgeons place a focus on alleviating pain, preventing worsening progression, and improving gait and mobility.
Although a very small number of surgeons claim to be able to remove all Lipedema fat, thereby “curing” the patient, there is no way to know if that is truly the case because there is no way to definitively say all Lipedema fat is gone, or if the underlying problem was fixed.
Other Surgical Considerations
Post-op care often includes compression, manual lymphatic drainage (MLD) and light exercise like walking to stimulate lymphatic vessel pumping.
Surgery can sometimes have a significant mental health impact on patients. It is important to have realistic expectations about recovery and surgical goals.
Adherance to pre-op and post-op protocols is important, and setting healthy routines before surgery should be advised (eating well, MLD, compression).
The lymphatics system and lymphatic dysfunction can impact anesthesia.
It is important to do careful research prior to electing surgery. Social media can be a useful tool to connect with other Lipedema patients who have shared their surgical experiences.
*While bariatric surgery has very limited (if any) effect on lipedematous tissue directly, non-lipedema fat and obesity can be reduced. Patients should be aware of this when they are considering which treatments to pursue.