Diagnosing Lipedema
Lipedema requires a clinical diagnosis, meaning there is not yet a standardized test such as bloodwork or imaging that can confirm the presence of Lipedema. Diagnosis should be reached in the context of a thorough patient history and physical exam.
Learn more about the patient history and interview and physical exam in these two videos and reference the Clinician’s Guide to Lipedema for more clinical diagnostic support.
Patient History
Clinicians should complete a detailed history with the patient, taking note if the following symptoms are reported:
Family history of similar body type
Difficulty losing fat in affected areas
Onset/worsening at time of hormonal change
Pain, tenderness, heaviness in affected areas
Fatigue
Brain fog
Easy tendency to bruise
Decreased functional ability (including mobility)
Decreased quality of life
History of joint issues
The following treatments have limited to no effect:
Elevation
Nutritional Interventions
Exercise
Diuretics
Bariatric Surgery
Physical Examination
The physical examination for a Lipedema diagnosis includes visual inspection and physical palpation. Clinicians may also complete the Stemmer sign test to assess for co-morbid Lymphedema. (See more below about the Stemmer sign test).
VISUAL INSPECTION
Bilateral, symmetrical fat accumulation that can appear in a combination of the legs, buttocks, hips, arms and/or lower trunk
Disproportion between upper and lower body
Lobules of fat may present at hips, medial knees, lateral malleoli, or above elbows
Presence of raised ridge/fold of fat, possibly a “cuff” at wrists and ankles
Presence of spider veins/varicosities
PALPATION
Presence of nodular and/or fibrotic texture in affected areas
Lipedema tissue texture can vary widely and be quite diverse. It may feel like fluffy fat with nodules embedded in it, have a dense, cement-like texture, feel granular or grainy, or even have a spongy texture
Nodules may feel like rice, peas, or walnuts
Fibrosis may feel dense, firm, woody, putty-like, cement-like, stringy, or spider-web like
Pain/tenderness in affected areas
Cutaneous hypothermia may be present
STEMMER SIGN TEST
Lipedema typically spares the hands/feet and presents with a negative Stemmer sign. However, a positive sign does not rule out Lipedema, and likely indicates the presence of concomitant Lymphedema. If both conditions are present, this is termed “Lipo-Lymphedema”.
Performing the test: Examiner pinches the dorsal skin proximal to the MTP joint of the second toe (or MCP joint of the second finger). If the examiner cannot create a fold of pinched skin, this results in a positive sign.
If you can pinch, the Stemmer sign is negative, and Lymphedema is likely not present.
If you cannot pinch, the Stemmer sign is positive, and Lymphedema is likely present.
Signs and Symptoms
Today, the most frequently cited components of a Lipedema diagnosis include:
Bilateral, symmetrical buildup of fat in extremities and/or lower trunk that is resistant to diet, exercise, or bariatric surgery
Feet/hands are typically spared, sometimes causing the appearance of an ankle or wrist “cuff”
Almost exclusively affects women
Complaints of pain, tenderness, heaviness, in affected areas
Fatigue
Starts or worsens at times of hormonal changes: puberty, pregnancy, or menopause
Easy bruising
Presence of nodular and/or fibrotic texture beneath the skin that can create an uneven, dimpled appearance
Edema and joint hypermobility may also be present
Download our free Clinician’s Guide to Lipedema
Our Clinician’s Guide outlines the latest diagnostic criteria, clinical signs, and care recommendations for clinicians to support Lipedema management.
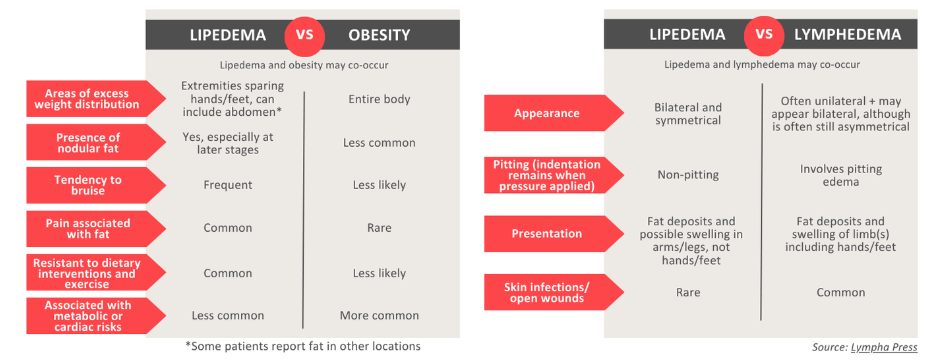
Differential Diagnosis
Photos, from left: Unlike obesity-related fat, Lipedema-related fat is not smooth but instead feels like rice, pea- or walnut-sized nodules; fat nodules extracted by Dr. Anne Dancey (UK); Lipedema fat removed via liposuction by Dr. Jason Emer (CA, USA).
See more about the different causes of leg swelling here.
Diagnostic Criteria May Vary
A Lipedema diagnosis and treatment plan may vary depending on the clinician and the country in which the patient is being seen. Several attempts have been made to build on the original descriptions of Lipedema that were first described in the 1940s. To date, six international guidelines and consensus statements with three other commonly cited clinical papers guide the identification of Lipedema in most clinical encounters. These include:
Diagnosing Lipedema in the Future
Although a Lipedema diagnosis requires the expertise of a skilled professional, this may be supported in the future by research that is currently leveraging our growing understanding of Lipedema biology to create tools that will help health care providers differentiate Lipedema from other similar conditions.
The Lipedema Foundation is actively working with patients and researchers to shorten the time to diagnosis and increase the certainty of any Lipedema diagnosis. Our research initiatives cross many technologies, and have highlighted specific areas where even simple advancements could pay enormous benefit to patients and the research that supports them. These include:
Genetics: Though there does not seem to be any single gene that causes Lipedema, it does tend to “run in families.” Current research is examining groups of genes that may work together to influence the risk of Lipedema.
Soft tissue imaging: Common imaging platforms such as MRI, Ultrasound, DEXA, and CT scans are being used to measure characteristic differences in Lipedema between tissue thickness, or ratios of elements like fat to muscle. Specialty MRI systems are currently being used to measure levels of tissue sodium. Other specialty systems like NIRFLI and lymphoscintigraphy are showing promise in their ability to map the structure and highlight function of lymphatic networks in Lipedema.
Surface imaging: Mapping the contours of the surface of the body may offer an ability to differentiate between conditions like lymphedema, obesity, and Lipedema. 3D scanning technologies are commonly used in some clinics, and may improve with increased access to Lipedema patients. Lipedema patients have often reported airport scanners (also known as millimeter wave imaging) have been singled out by patients as a commonly encountered technology. This could lead to a possible Lipedema imaging tool.
Changes in biophysics of tissue: Lipedema may change the elasticity of tissue or alter their natural electrical conductance that can be observable through techniques like bioimpedance. Although easy bruising is often reported as a symptom of Lipedema, biophysical tests to measure the fragility of capillaries remain to be tested with the condition.
Funding Research to Aid Diagnosis
The Lipedema Foundation is actively funding research to develop tools to aid Lipedema diagnosis. These technologies range from imaging and clinical laboratory tests that might one day be used to diagnose a patient directly, to genetic approaches that might help understand a person’s risk for developing Lipedema.
With this cutting edge research, we are working with patients and researchers to shorten the time and increase the certainty behind any Lipedema diagnosis.