LF is at the Boston Lymphatics Symposium
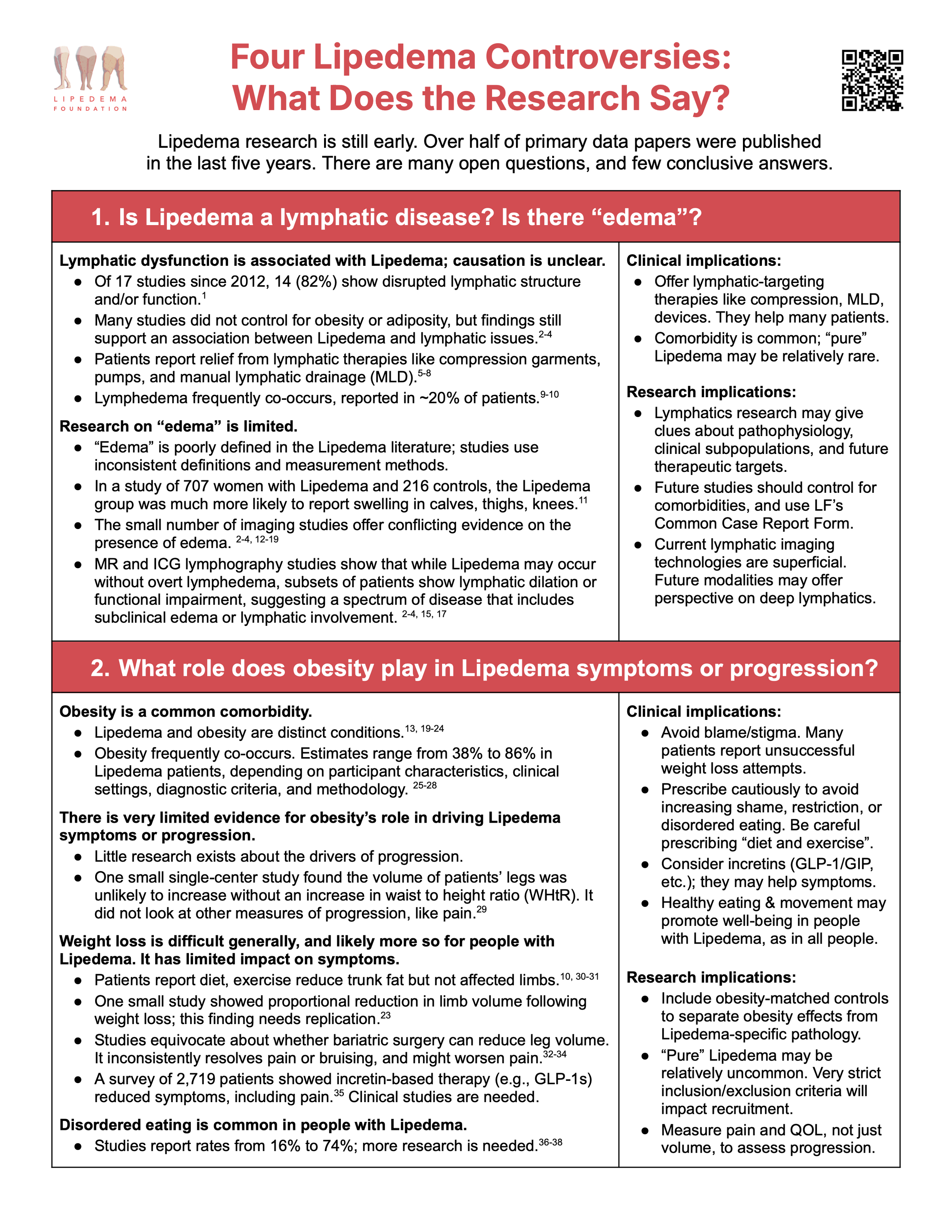
Four Lipedema Controversies: What does the Research Say?
-
Eakin, G. S., & Peterson, S. (2023, May). Lipedema: A current understanding of its pathology and natural history (Version 1). Lipedema Foundation.
Crescenzi R, Donahue PMC, Garza M, et al. Subcutaneous adipose tissue edema in lipedema revealed by noninvasive 3T MR lymphangiography. J Magn Reson Imaging. 2022;57(2):598-608. doi: 10.1002/jmri.28281
Zaleska MT, Olszewski WL, Krzesniak NE. Lower Limb Lipedema-Superficial Lymph Flow, Skin Water Concentration, Skin and Subcutaneous Tissue Elasticity. Lymphat Res Biol. 2023 Feb;21(1):60-69. doi: 10.1089/lrb.2022.0010
Rasmussen JC, Aldrich MB, Fife CE, Herbst KL, Sevick-Muraca EM. Lymphatic function and anatomy in early stages of lipedema. Obesity (Silver Spring). 2022;30(7):1391-1400. doi: 10.1002/oby.23458
Lipedema Foundation. (2022). Learning by listening: First look—Early findings from the Lipedema Foundation Registry survey. Lipedema Foundation.
Donahue, P. M. C., Crescenzi, R., Petersen, K. J., Garza, M., Patel, N., Lee, C., Chen, S.-C., & Donahue, M. J. (2022). Physical Therapy in Women with Early Stage Lipedema: Potential Impact of Multimodal Manual Therapy, Compression, Exercise, and Education Interventions. Lymphatic Research and Biology, 20(4), 382–390. https://doi.org/10.1089/lrb.2021.0039
Czerwińska, M., Gruszecki, M., Rumiński, J., & Hansdorfer-Korzon, R. (2024). Evaluation of the Effectiveness of Compression Therapy Combined with Exercises Versus Exercises Only Among Lipedema Patients Using Various Outcome Measures. Life (Basel, Switzerland), 14(11), 1346. https://doi.org/10.3390/life14111346
Herbst, K. L., Zelaya, C., Sommerville, M., Zimmerman, T., & McHutchison, L. (2025). An Advanced Pneumatic Compression Therapy System Improves Leg Volume and Fluid, Adipose Tissue Thickness, Symptoms, and Quality of Life and Reduces Risk of Lymphedema in Women with Lipedema. Life, 15(5), 725. https://doi.org/10.3390/life15050725
Forner-Cordero et al., “Prevalence of Clinical Manifestations and Orthopedic Alterations in Patients with Lipedema.” https://journals.librarypublishing.arizona.edu/lymph/article/id/4838/, Lymphology 54 (2021) 170-181
Grigoriadis D, Sackey E, Riches K, van Zanten M, Brice G, et al. (2022) Investigation of clinical characteristics and genome associations in the ‘UK Lipoedema’ cohort. PLOS ONE 17(10): e0274867. https://doi.org/10.1371/journal.pone.0274867
Aday, A. W., Donahue, P. M., Garza, M., Crain, V. N., Patel, N. J., Beasley, J. A., Herbst, K. L., Beckman, J. A., Taylor, S. L., Pridmore, M., Chen, S.-C., Donahue, M. J., & Crescenzi, R. (2023). National survey of patient symptoms and therapies among 707 women with a lipedema phenotype in the United States. Vascular Medicine (London, England), 1358863X231202769.
Hirsch, T., Schleinitz, J., Marshall, M., & Faerber, G. (2018). Ist die Differenzialdiagnostik des Lipödems mittels hochauflösender Sonografie möglich? Phlebologie, 47(04), 182–187. https://doi.org/10.12687/phleb2431-4-2018
Crescenzi, R., Marton, A., Donahue, P. M. C., Mahany, H. B., Lants, S. K., Wang, P., Beckman, J. A., Donahue, M. J., & Titze, J. (2018). Tissue Sodium Content is Elevated in the Skin and Subcutaneous Adipose Tissue in Women with Lipedema. Obesity (Silver Spring, Md.), 26(2), 310–317. https://doi.org/10.1002/oby.22090
Crescenzi, R., Donahue, P. M. C., Petersen, K. J., Garza, M., Patel, N., Lee, C., Beckman, J. A., & Donahue, M. J. (2020). Upper and Lower Extremity Measurement of Tissue Sodium and Fat Content in Patients with Lipedema. Obesity (Silver Spring, Md.), 28(5), 907–915. https://doi.org/10.1002/oby.22778
Buso, G., Favre, L., Maufus, M., Honorati, M., Lessert, C., Depairon, M., Raffoul, W., Tomson, D., & Mazzolai, L. (2021). Indocyanine green lymphography as novel tool to assess lymphatics in patients with lipedema. Microvascular Research, 104298. https://doi.org/10.1016/j.mvr.2021.104298
Mackie, H., Thompson, B. M., Suami, H., Heydon-White, A., Blackwell, R., Tisdall Blake, F., & Koelmeyer, L. A. (2023). Differentiation of lipoedema from bilateral lower limb lymphoedema by imaging assessment of indocyanine green lymphography. Clinical Obesity, e12588. https://doi.org/10.1111/cob.12588
Cellina, M., Gibelli, D., Soresina, M., Menozzi, A., Martinenghi, C., Panzeri, M., & Oliva, G. (2020). Non-contrast MR Lymphography of lipedema of the lower extremities. Magnetic Resonance Imaging, 71, 115–124. https://doi.org/10.1016/j.mri.2020.06.010
Felmerer, G., Stylianaki, A., Hollmén, M., Ströbel, P., Stepniewski, A., Wang, A., Frueh, F. S., Kim, B.-S., Giovanoli, P., Lindenblatt, N., & Gousopoulos, E. (2020). Increased levels of VEGF-C and macrophage infiltration in lipedema patients without changes in lymphatic vascular morphology. Scientific Reports, 10(1), 10947. https://doi.org/10.1038/s41598-020-67987-3
Von Atzigen, J., Burger, A., Grünherz, L., Barbon, C., Felmerer, G., Giovanoli, P., Lindenblatt, N., Wolf, S., & Gousopoulos, E. (2023). A Comparative Analysis to Dissect the Histological and Molecular Differences among Lipedema, Lipohypertrophy and Secondary Lymphedema. International Journal of Molecular Sciences, 24(8), 7591. https://doi.org/10.3390/ijms24087591
Ishaq, M., Bandara, N., Morgan, S., Nowell, C., Mehdi, A. M., Lyu, R., McCarthy, D., Anderson, D., Creek, D. J., Achen, M. G., Shayan, R., & Karnezis, T. (2021). Key signaling networks are dysregulated in patients with the adipose tissue disorder, lipedema. International Journal of Obesity, 1–13. https://doi.org/10.1038/s41366-021-01002-1
Kruppa, P., Gohlke, S., Łapiński, K., Garcia-Carrizo, F., Soultoukis, G. A., Infanger, M., Schulz, T. J., & Ghods, M. (2023). Lipedema stage affects adipocyte hypertrophy, subcutaneous adipose tissue inflammation and interstitial fibrosis. Frontiers in Immunology, 14. https://www.frontiersin.org/articles/10.3389/fimmu.2023.1223264
Al-Ghadban, S., Isern, S. U., Herbst, K. L., & Bunnell, B. A. (2024). The Expression of Adipogenic Marker Is Significantly Increased in Estrogen-Treated Lipedema Adipocytes Differentiated from Adipose Stem Cells In Vitro. Biomedicines, 12(5), 1042. https://doi.org/10.3390/biomedicines12051042
Cifarelli, V., Smith, G. I., Gonzalez-Nieves, S., Samovski, D., Palacios, H. H., Yoshino, J., Stein, R. I., Fuchs, A., Wright, T. F., & Klein, S. (2024). Adipose tissue biology and effect of weight loss in women with lipedema. Diabetes, db240890. https://doi.org/10.2337/db24-0890
Straub, L. G., Funcke, J.-B., Joffin, N., Joung, C., Al-Ghadban, S., Zhao, S., Zhu, Q., Kruglikov, I. L., Zhu, Y., Langlais, P. R., Gordillo, R., Herbst, K. L., & Scherer, P. E. (2025). Defining lipedema’s molecular hallmarks by multi-omics approach for disease prediction in women. Metabolism, 156191. https://doi.org/10.1016/j.metabol.2025.156191
Erbacher, G., & Bertsch, T. (2020). Lipoedema and pain: What is the role of the psyche? Results of a pilot study with 150 patients with lipoedema. Phlebologie, 49, 305–316. https://doi.org/10.1055/a-1238-6657
Patton, L.; Ricolfi, L.; Bortolon, M.; Gabriele, G.; Zolesio, P.; Cione, E.; Cannataro, R. Observational Study on a Large Italian Population with Lipedema: Biochemical and Hormonal Profile, Anatomical and Clinical Evaluation, Self-Reported History. Int. J. Mol. Sci. 2024, 25, 1599. https://doi.org/10.3390/ijms25031599
Luta X, Buso G, Porceddu E, Psychogyiou R, Keller S, et al. (2025) Clinical characteristics, comorbidities, and correlation with advanced lipedema stages: A retrospective study from a Swiss referral centre. PLOS ONE 20(3): e0319099. https://doi.org/10.1371/journal.pone.0319099
Ghods M, Georgiou I, Schmidt J, Kruppa P. Disease progression and comorbidities in lipedema patients: A 10-year retrospective analysis. Dermatol Ther. 2020 Nov;33(6):e14534. doi: 10.1111/dth.14534. Epub 2020 Nov 22. PMID: 33184945.
I, Forner-Cordero, and Muñoz-Langa J. “Is Lipedema a Progressive Disease?” Vascular Medicine (London, England) 30, no. 2 (2025): 205–12. https://doi.org/10.1177/1358863X241306415.
Amato, Alexandre Campos Moraes, Fernando Campos Moraes Amato, Juliana Lelis Spirandeli Amato, and Daniel Augusto Benitti. “Lipedema Prevalence and Risk Factors in Brazil.” Jornal Vascular Brasileiro 21 (2022): e20210198. https://doi.org/10.1590/1677-5449.202101981.
Fetzer, A., & Fetzer, S. (2014). Lipoedema UK big survey 2014: Research report. Lipoedema UK. https://www.lipoedema.co.uk/wp-content/uploads/2016/04/UK-Big-Surey-version-web.pdf
Fink, T., Schreiner, S., Marjanovic, G., et al. (2021). Leg volume in patients with lipoedema following bariatric surgery. Visceral Medicine, 37, 206–211. https://doi.org/10.1159/000514842
Cornely ME, Hasenberg T, Cornely OA, Ure C, Hettenhausen C, Schmidt J. Persistent lipedema pain in patients after bariatric surgery: a case series of 13 patients. Surg Obes Relat Dis. 2022
Zevallos, A., Schmidt, J., Thaher, O., Bausch, D., & Pouwels, S. (2025). Lipedema after bariatric and metabolic surgery: A scoping review. Obesity Surgery, 35(8), 3241–3245. https://doi.org/10.1007/s11695-025-08021-1
Cochrane, JC, et al. GLP-1 and GLP-1/GIP Receptor Agonist Medication Use and Self-Reported Outcomes in Individuals with Lipedema: Results from a Large Online Survey (in preparation)
Kraus, R. H. (2015). Alles über das Lipödem [All about lipedema]. Lymphe & Gesundheit, 2015(1), 1–9.
Clarke, C., Kirby, J. N., Smidt, T., & Best, T. (2022). Stages of lipoedema: Experiences of physical and mental health and health care. Quality of Life Research. https://doi.org/10.1007/s11136-022-03216-w
Kunzová, M. (2026). Disordered eating risk and well-being in women with lipedema. Frontiers in Global Women’s Health, 7. https://doi.org/10.3389/fgwh.2026.1720708
Rapprich et al., “Treatment of Lipoedema Using Liposuction.” Phlebologie 2015; 44(03): 121-132 DOI: 10.12687/phleb2265-3-2015
NORD (National Organization for Rare Disorders) https://rarediseases.org/wp-content/uploads/2016/11/NORD-Lipedema-article-1.pdf
ILA (International Lipoedema Association) https://theila.net/8-myths-about-lipoedema/myth-lipedema-is-a-common-disease/
Forner-Cordero I, Forner-Cordero A, Szolnoky G. Update in the management of lipedema. Int Angiol. 2021 Aug;40(4):345-357. doi: 10.23736/S0392-9590.21.04604-6. Epub 2021 Apr 19. PMID: 33870676.
Falck J, Rolander B, Nygårdh A, Jonasson LL, Mårtensson J. Women with lipoedema: a national survey on their health, health-related quality of life, and sense of coherence. BMC Womens Health. 2022 Nov 18;22(1):457. doi: 10.1186/s12905-022-02022-3. PMID: 36401222; PMCID: PMC9673372.
Bauer AT, von Lukowicz D, Lossagk K, Aitzetmueller M, Moog P, Cerny M, Erne H, Schmauss D, Duscher D, Machens HG. New Insights on Lipedema: The Enigmatic Disease of the Peripheral Fat. Plast Reconstr Surg. 2019 Dec;144(6):1475-1484. doi: 10.1097/PRS.0000000000006280. PMID: 31764671.
Dinnendahl, R., Tschimmel, D., Löw, V., Cornely, M., & Hucho, T. (2023). Non-obese lipedema patients show a distinctly altered quantitative sensory testing profile with high diagnostic potential. PAIN Reports, 9(3), e1155. https://doi.org/10.1097/PR9.0000000000001155
Dudek, J.E., Białaszek, W. & Ostaszewski, P. Quality of life in women with lipoedema: a contextual behavioral approach. Qual Life Res 25, 401–408 (2016). https://doi.org/10.1007/s11136-015-1080-x
Chakraborty A, Crescenzi R, Usman TA, Reyna AJ, Garza ME, Al-Ghadban S, Herbst KL, Donahue PMC, Rutkowski JM. Indications of Peripheral Pain, Dermal Hypersensitivity, and Neurogenic Inflammation in Patients with Lipedema. Int J Mol Sci. 2022 Sep 7;23(18):10313. doi: 10.3390/ijms231810313. PMID: 36142221; PMCID: PMC9499469.
Podda M, Kovacs M, Hellmich M, Roth R, Zarrouk M, Kraus D, Prinz-Langenohl R, Cornely OA. A randomised controlled multicentre investigator-blinded clinical trial comparing efficacy and safety of surgery versus complex physical decongestive therapy for lipedema (LIPLEG). Trials. 2021 Oct 30;22(1):758. doi: 10.1186/s13063-021-05727-2. PMID: 34717741; PMCID: PMC8557553.
Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, Keefe FJ, Mogil JS, Ringkamp M, Sluka KA, Song XJ, Stevens B, Sullivan MD, Tutelman PR, Ushida T, Vader K. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020 Sep 1;161(9):1976-1982. doi: 10.1097/j.pain.0000000000001939. PMID: 32694387; PMCID: PMC7680716.
Daftuar, F. et al. Lipedema Research Roadmap (2023) Lipedema Foundation
Erden, E., Turk, A. C., Erden, E., Yetim, S., & Borman, P. (2025). The incidence of neuropathic pain and its impact on quality of life in patients with lipedema. Irish Journal of Medical Science, 194(5), 1829–1835. https://doi.org/10.1007/s11845-025-04024-0
Suggested reading list to prepare for the conference
Cifarelli V. Lipedema: Progress, Challenges, and the Road Ahead. Obes Rev. Published online May 27, 2025:e13953. doi:10.1111/obr.13953
Rabiee A. Lipedema and adipose tissue: current understanding, controversies, and future directions. Front Cell Dev Biol. 2025;13. doi:10.3389/fcell.2025.1691161
Kruppa P, Crescenzi R, Faerber G, et al. Lipedema World Alliance Delphi Consensus-Based Position Paper on the Definition and Management of Lipedema: Results from the 2023 Lipedema World Congress in Potsdam. Nat Commun. 2026;17(1):427. doi:10.1038/s41467-025-68232-z
Funcke JB, Scherer PE, Straub LG. Lipedema: a chronic adipose tissue disease. Trends in Molecular Medicine. Published online December 2025:S1471491425002850. doi:10.1016/j.molmed.2025.11.005
Come find us at BLS!
Collecting data?
Use our Common Case Report Form and help standardize data collection in Lipedema.
Lipedema Foundation Biobank
The Lipedema Foundation Biobank is a new initiative created to support research into the causes, diagnosis, and treatment of Lipedema. By collecting and securely storing biospecimens and health information from individuals with Lipedema and related conditions, the Biobank will become a resource for scientists working to better understand this complex disease.
To request samples from the biobank, reach out to biobank@lipedema.org
Have great ideas about how we should use biobank samples?
About the Foundation
The Lipedema Foundation is a private, non-fundraising organization established in 2015 to define, diagnose and develop treatments for Lipedema. It has awarded more than $13.6 million to date, funding 64 research studies with partners at 55 institutions in 10 countries. In 2025, the Lipedema Foundation launched the Lipedema Foundation Biobank to support research into the causes, diagnosis, and treatment of Lipedema, and continues to maintain the Lipedema Foundation Registry. Meet the team!
Research Resources
Review Lipedema Foundation’s Lipedema Research Roadmap, which recommends action to grow and strengthen Lipedema Research.
Lipedema Foundation has funded $13.6M in research, across 64 studies with research partners at 55 institutions in 10 countries. Learn about our recent projects.
Looking for Lipedema research papers? Our on-line Legato Library makes it easy to search for Lipedema research by keyword, topics, and more.
The First Look Report features the findings of the Registry survey from data provided by 521 participants with Lipedema.
Clinician & Patient Resources
Access the Clinician’s Guide, information about diagnosis and ICD-codes, treatment information, and many more resources on our For Clinicians page.
Request free print copies here.
Access our Lipedema Care & Treatments Options graphic and details regarding treating Lipedema here.
The LF Provider Directories are designed to help people with Lipedema, their healthcare providers, and others identify professionals who have told us they treat and/or diagnose Lipedema in their clinical practice. Access our Therapist Directory and our Diagnosing Clinician Directory.
Sign up for the Lipedema Foundation Registry! Participation in our Registry helps support scientific research to improve the life of Lipedema patients.
Want to participate in research studies? If you wish to learn about clinical research studies and patient surveys that are seeking Lipedema patients, check out our LegWork Clinical Trial Finder.
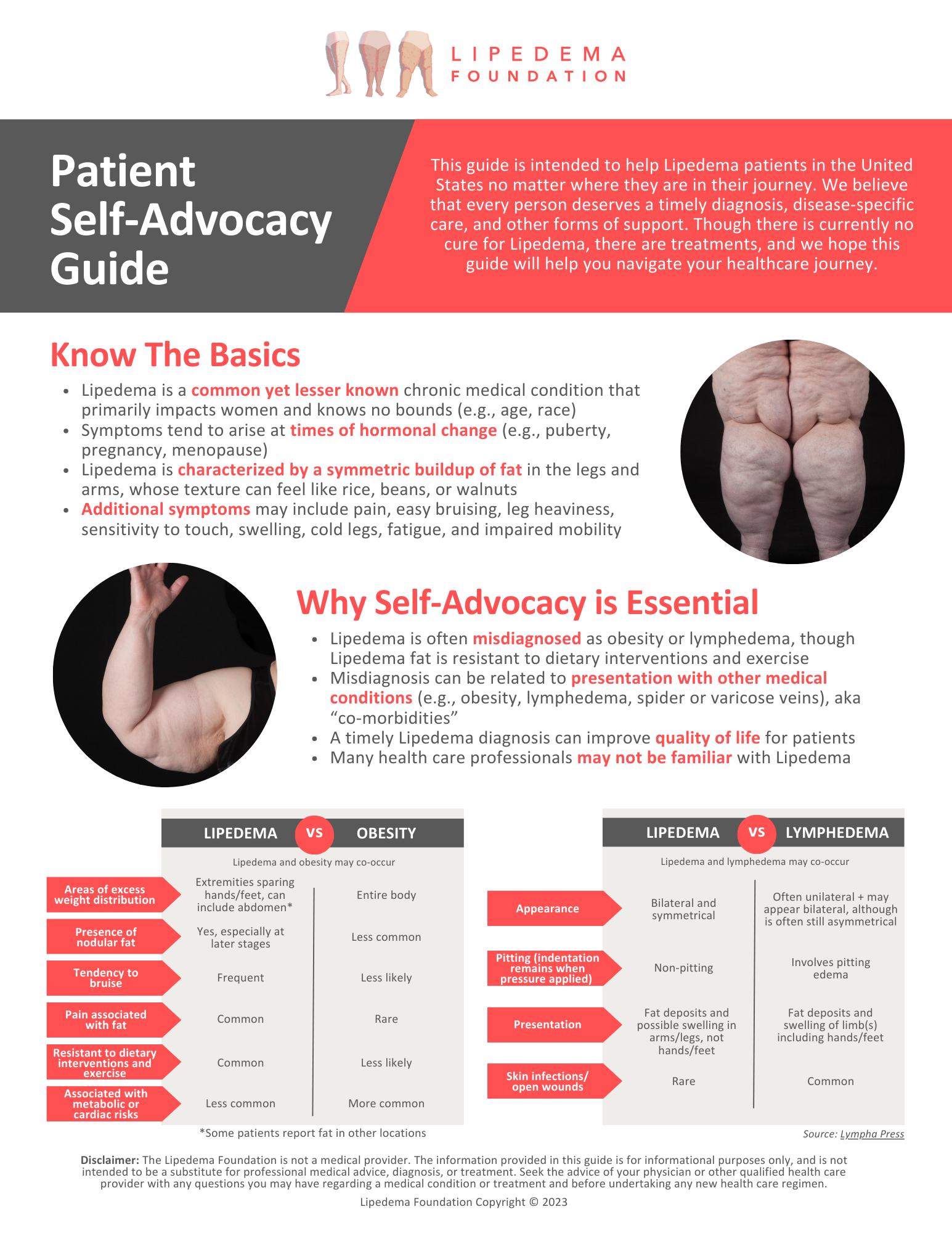
Our Patient Self-Advocacy Guide is intended to help Lipedema patients as they navigate their healthcare journey. Though there is currently no cure for Lipedema, we believe that every person deserves a timely diagnosis, disease-specific care, and other forms of support.
Lipedema Education Resources
View Unmasking Lipedema in Obesity: Key Diagnostic Tips & Proven Management Strategies for Better Care, a recorded session from OMA. This is offered for free CME credit to those who are eligible.
Download or order free copies of Lipedema Foundation Brochure, which features key questions that patients may have about Lipedema. Download or order free brochures or Clinician’s Guides here.
Check out our Lipedema Photo Stories and photo gallery with >500 photos of Lipedema.
The ‘What is LIpedema?’ video features descriptions about Lipedema symptoms, diagnosis challenges, and related disorders.